|
Evan's syndrome is an extremely rare autoimmune disorder. The immune system destroys the body's red blood cells, platelets, and/or white blood cells.
Those who suffer from this illness may have the following:
What causes Evan's syndrome? Exact causes are unknown, but researchers believe that the syndrome is a dysregulation of the immune system. What are the symptoms of Evan's syndrome? Symptoms vary from person to person, as with any disease. Symptoms may vary according to what blood cells may be affected. Some of the most common symptoms associated with this syndrome include:
How is Evan's syndrome diagnosed? Your doctor will be checking your symptoms and sending you for blood tests. In some cases, your doctor may order a bone marrow aspiration procedure in order to make a definitive diagnosis. How is Evan's syndrome treated? Treatment depends on your symptoms and severity of your condition. Those who have severe anemia may be hospitalized and treated with blood transfusions. Afterward, patients will be treated with corticosteroids and IV immune globulin. Immunosuppressive drugs may also be considered as a form of treatment. Those who do not respond to these treatments may be recommended for rituximab or splenectomy therapies. Those who have a very severe case of Evan's syndrome may be recommended for stem cell transplantation. Closing remarks It is important for those living with Evan's syndrome to be carefully monitored by their doctor. While you may go through periods of remission, going without medication, and not communicating with your doctor, can put you at serious risk. Evan's syndrome has a history of being a fatal disease. Keep in contact with your doctor, and never discontinue your medication UNLESS your doctor says so.
0 Comments
CREST syndrome is a subtype of Scleroderma (hardening of the skin). With CREST syndrome, skin changes happen in the lower arms and legs. In some cases, it may occur on the face and throat. This condition has also been known to affect the GI tract in some patients.
While problems with CREST syndrome may be on the mild side, in rare cases, the disease can damage the heart and lungs, causing life-threatening results. CREST syndrome is considered an autoimmune disorder, due to the fact that the immune system causes an overproduction of too much collagen. This can build up on the skin, and in some cases, internal organs, causing a disruption in normal functioning. What are the risk factors of CREST Syndrome? Women are more likely to have this condition than men. This condition is said to affect people of color more often than Caucasians. Individuals with a family history of autoimmune disorders, such as Rheumatoid Arthritis, Lupus, or Hashimoto's disease, are at an increased risk for CREST syndrome. What are the symptoms of CREST syndrome? Individuals who have at least two of the following symptoms may have this form of Scleroderma:
How is CREST syndrome diagnosed? CREST syndrome is a complex autoimmune disorder, and can be difficult to diagnose. Your doctor will ask you about your symptoms and family history. From there, your doctor may order blood tests and a skin biopsy in order to definitively diagnose you. In some cases, your doctor may order tests to look at your GI tract, lungs, and heart, in order to spot any complications from the disease. How is CREST syndrome treated? While there is no known cure for CREST syndrome, there are several different ways that the symptoms can be treated. These treatments include:
Your doctor may order various types of therapy to help you maintain strength and flexibility. Some of these therapies include:
In severe cases, surgery may be recommended. Closing remarks Just like with Scleroderma, CREST causes physical changes that can affect your self-esteem. If you find yourself suffering from some depression because of this disease, please seek help from a counselor. Talking to a counselor is not shameful at all. They can help you come to terms with your illness and provide you coping techniques to help you get through your day. Also, look into support groups. In support groups, you can meet others who are suffering from similar issues. Support groups help you feel less alone. 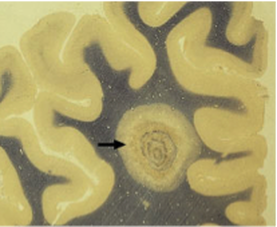 Balo's disease is a subtype of Multiple Sclerosis. Like MS, Balo's disease consists of myelin damage in the nervous system. As you might remember from my MS post, myelin is made up of fatty substances that envelope and protect nerve fibers in the spinal cord and brain. Myelin is essential for correct neurological functioning. What makes Balo's disease somewhat different from MS is that damage to the myelin is circular-shaped. Who is at risk for Balo's Disease? As with MS, Balo's disease is considered an autoimmune disorder. With Balo's disease, not only does the immune system attack healthy tissue, it also attacks healthy cells as well. While a lot is still unknown about Balo's disease, researchers do know that the following increase your risk for Balo's disease:
Symptoms of Balo's Disease
In very rare cases, Balo's disease may not show any symptoms. Diagnosis of Balo's Disease If you show signs of Balo's disease, your doctor will order an MRI of the brain and spinal cord. He or she will be looking for circular rings on damaged myelin. Damage is often in a pattern, alternating between undamaged myelin and damaged myelin. Your doctor may order more tests to further evaluate you. These tests include:
Treatment for Balo's Disease Once diagnosed, your doctor will begin treating you. There are two ways to treat Balo's Disease:
Closing Remarks There is no cure for Balo's Disease, and it can be an unpredictable disease to treat and to provide a prognosis. While medication and therapy can help with the symptoms, it cannot stop the progression of the disease. The good news is people can survive this disease, and enter remission. It is important for those with Balo's Disease to work alongside their doctors and to adhere to the treatment plan that both of you have agreed upon. 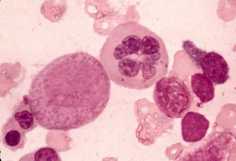 Aplastic Anemia is a rare blood disorder in which the bone marrow does not make enough new blood cells. When it comes to normal anemia, the individual does not produce enough red blood cells. With Aplastic Anemia, the individual does not make enough of all types of blood cells, this includes white blood cells and platelets. The life span of red blood cells is around 120 days. White blood cells live less than one day, and platelets live around 6 days. All of these blood cells must constantly reproduce and make new cells in order for the body to function as it should. When the body is unable to make new blood cells, several health problems could occur. What causes Aplastic Anemia? The cause can be either acquired or inherited. Individuals who acquire Aplastic Anemia may have done so by the following:
Who is 'at risk' for Aplastic Anemia?
Symptoms of Aplastic Anemia Those who have a low red blood cell count may experience fatigue, dizziness, shortness of breath, pale skin, chest pain, coldness in hands and feet, irregular heartbeat. Those who have a low white blood count may experience fever, infections, and flu symptoms that may linger for a long time. Those who have a low platelet count may experience nosebleeds, bloody stools, and bleeding gums. How is Aplastic Anemia diagnosed? If your physician suspects that you may have Aplastic Anemia, they may refer you to a hematologist for further evaluation. Your doctor will ask about your medical and family history. They will inquire about your symptoms, and conduct a physical examination. Next, your doctor will order a blood test and will look at your complete blood count. Other tests include:
Treatment for Aplastic Anemia Treatments for Aplastic Anemia may include:
**I included Aplastic Anemia in this series due to the disorder's relationship with autoimmune disorders. It is important for those of us with autoimmune diseases, specifically those with Lupus and RA, to know what we are at risk for if we don't adhere to our treatments.** If you suspect that you might have Aplastic Anemia, contact your doctor right away. 
Sarcoidosis is a inflammatory condition that impacts the lungs and lymph nodes. However, it has been known to affect multiple organs in the human body.
Individuals who have this disease exhibit abnormal masses, or granulomas. These granulomas are made up of inflamed tissues which have formed in various organs in the body. The granulomas may change the normal structure and functioning of these affected organs. The onset of Sarcoidosis is said to begin between the ages of 20 and 40. Women are often diagnosed more than men. What is the cause of Sarcoidosis? A root cause for Sarcoidosis is unknown. What is known is that it is an autoimmune disease. Researchers are still studying how this condition can move from one part of the body, to the other. Symptoms of Sarcoidosis
How is Sarcoidosis diagnosed? Because there is no root way to diagnose this condition, you doctor will review your medical history and examine you. If your doctor suspects that you may have Sarcoidosis, the following exams may be ordered:
Treatment for Sarcoidosis This condition has no cure, but symptoms can be treated by maintaining good health, and drug treatment. Drug treatments may include:
In many cases, the disease may come and go without you even noticing. For 20%-30% of patients, there may be some permanent lung damage. For a small percentage of people, this disease is a chronic condition. In very rare cases, complications from Sarcoidosis can be fatal. If you suspect that you may have Sarcoidosis, contact your primary doctor.  Autonomic neuropathy is a condition that occurs when nerves in charge of bodily functions are damaged. Areas affected include digestion, bladder functioning, blood pressure, and sexual functioning. The damaged nerves interfere with messages being sent from the brain to other organs across the autonomic nervous system. Areas involved include sweat glands, heart, and blood vessels. Causes of Autonomic Neuropathy Diabetes is the most common cause of Autonomic neuropathy, but other illnesses can cause this condition as well. These illnesses include:
Other causes of Autonomic Neuropathy include:
Symptoms of Autonomic Neuropathy Symptoms vary based on what nerves are affect. The most common symptoms include the following:
How is Autonomic Neuropathy diagnosed? The type of testing for this condition depends on your symptoms and risk factors. Autonomic Neuropathy is known to be a possible complication for several diseases. If you have risk factors and symptoms of this condition, your doctor may perform a physical exam and ask you what symptoms you are experiencing. If you have symptoms of Autonomic neuropathy but do not have risk factors for the condition, your doctor will perform a physical exam, talk about your medical history, and order the following tests:
Treatment for Autonomic Neuropathy Treatment may include the following:
Closing remarks: While this condition isn't an autoimmune disease in itself, it is one that those of us with autoimmune disease should be aware of. If you exhibit any of the above symptoms, contact your doctor immediately. Myositis is a term used to describe inflammation in the muscles. This condition may be caused by injury, infection, or autoimmune conditions.
There are several categories of Myositis:
Symptoms of Myositis
How is Myositis diagnosed? If your doctor suspects that you may have myositis, he may order one or more of the following tests:
Treatment for Myositis Once a diagnosed for Myositis has been determined, your doctor will begin treating you. Treatment consists of the following:
Closing remarks While Myositis isn't considered an autoimmune condition, those of us with autoimmune diseases, such as the ones listed above, are at a higher risk for it. It is important that we adhere to the treatment our doctors have provided for us so this condition does not develop. If you suspect that you may have Myositis, contact your doctor right away. 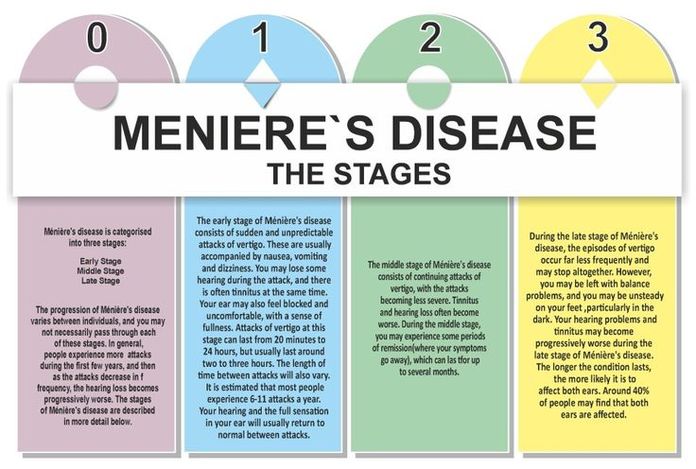 Meniere's disease is an inner ear issue that can impact one's balance and hearing. It typically impacts one ear at a time. However, it can develop in the other ear over time. Individuals are usually diagnosed with Meniere's after age 40, but it can develop at any age. What causes Meniere's? As with many of the conditions that I've discussed, the cause of Meniere's is unknown. Experts believe that it might be related to fluid in the inner ear called endolymph. In people who have Meniere's, there is too much endolymph in the inner ear. This causes pressure in the inner ear, creating issues with balance. Experts have two theories as to why this happens:
Is Meniere's disease autoimmune? While Meniere's itself isn't an autoimmune disease, those of us who suffer from autoimmune disease are at a higher than normal risk for Meniere's. Symptoms of Meniere's disease
Those with Meniere's may experience what is called "drop attacks." Drop attacks are a sudden fall when standing or walking. It happens with no warning to the sufferer. How is Meniere's diagnosed? If you suspect that you have Meniere's, your doctor will do a physical exam, checking the ears, eyes, and nervous system. He will also ask a wide variety of questions about your symptoms. Other tests might include:
How is Meniere's treated? Meniere's disease cannot be cured, but it can be treated. Your doctor will prescribe you medications to help with the vertigo symptoms. A diuretic medication may be prescribed as well. In severe cases of the disease, surgery may be recommended.  Kawasaki disease affects 4,000 children in the United States each year. Kawasaki disease is a rare autoimmune condition that causes inflammation in the blood vessels. This disease is known to affect only children. The disease was first discovered in Japan, and is diagnosed in boys more than girls. The onset of Kawasaki disease occurs in children younger than 5 years of age. While the root cause of Kawasaki disease is not yet known, experts believe that it is an autoimmune disorder. Kawasaki disease is known to affect the lymph nodes, blood vessel walls, heart, and mucous membranes. Symptoms of Kawasaki disease -Fever of 102 degrees that lasts more than 5 days -Swollen hands and feet -Bloodshot eyes -Joint pain -Peeling skin on the hands, feet, and in the genital area -Swollen lymph nodes -Nausea -Coughing -Diarrhea -Runny nose Testing for Kawasaki disease Doctors will usually diagnose the symptoms the child is experiencing. Doctors may order tests for further evaluation of the child. Some of these tests include: -Blood tests -Chest X-ray -C-reactive protein -Echocardiogram -Electrocardiogram -Urinalysis Treatment for Kawasaki disease Children with Kawasaki disease require hospitalization. Treatment would have to be started right away in order to prevent complications in the heart and arteries. Your child will be hooked up to an IV and will be given gamma globulin at high doses. Most children experience improvement within 24 hours. It is important to note that 1 in 4 children may develop problems with their coronary arteries, even after treatment. Most children do recover from this disease when it is caught early. Further research is being done in order to better understand and treat this disease.  1 in every 300,000 children in the United States is affected by Juvenile Arthritis. Juvenile Arthritis is an "umbrella term" used to describe a variety of autoimmune conditions that affect children under the age of 16. The various types of Juvenile Arthritis share a wide variety of symptoms, such as joint swelling, pain, warmth, and redness. Some types of JA affect the musculoskeletal system. Others may affect the eyes, muscles, skin, and gastrointestinal tract. Types of Juvenile Arthritis Types of JA include the following: -Juvenile Idiopathic Arthritis -Juvenile Lupus -Juvenile Scleroderma -Fibromyalgia What causes Juvenile Arthritis? While a cause for Juvenile Arthritis is still unknown, some suggest genetics may play a key factor. How is JA diagnosed? The journey to being diagnosed can be quite lengthy, as doctors want to be absolutely certain in their diagnosis. Your child will undergo a physical exam and he or she will look at your child's medical history. From there, your doctor will send you for various tests to help him or her with the diagnosis. Treatment for JA There is no cure for Juvenile Arthritis. However, an early diagnosis and treatment can help your child into remission. The goal of JA treatment is to reduce inflammation, manage pain, and help improve your child's quality of life. Children with JA have a treatment plan that consists of medication, eye care, physical activity, and dietary education. To find out more about Juvenile Arthritis, visit KidsGetArthritisToo. |
Archives
|
©2017-2024


 RSS Feed
RSS Feed
